Category: Physiology
Broken Heart Syndrome: Dying From Heartache
“Somehow, heartbreak feels good in a place like this.” —Nicole Kidman
When looking for love, heartbreak is always a risk, but you might not realize that a broken heart can be more than an emotional wound.
Most people, after feeling like their heart’s been torn out and put into a blender, manage to piece themselves back together in time. But for some, moving on feels impossible. And for fewer still, the pain becomes a crushing weight that builds until their heartbeat slows, breathing fades and eyes close, never to open again.
This brings us to broken heart syndrome, a medical condition as fascinating as it is deadly. If you’re worried about your own health, stop here and talk to a medical professional. But if you’re drawn to strange and unsettling conditions from the world of medicine, read on.
What Is Broken Heart Syndrome?
Broken heart syndrome seems like something out of a Shakespearean tragedy. As it turns out, broken heart syndrome — also called stress-induced cardiomyopathy or takotsubo syndrome — is a real heart condition characterized by sudden chest pain, shortness of breath, sweating and dizziness.
Sounds like a heart attack, right? While the symptoms are eerily similar, an episode of broken heart syndrome is temporary and won’t cause lasting damage if treated. But without medical attention, a sufferer’s heart muscle can weaken, leading to serious complications like:
- Congestive heart failure
- Dangerous heart rhythm abnormalities
- Low blood pressure
- Shock
What Causes Broken Heart Syndrome?
Often, it’s emotional stress: a painful breakup or the death of a loved one. But excitement from, say, being in a heated argument or watching a favorite sports team lose in overtime can also trigger the surge of stress hormones that lead to broken heart syndrome. There are also physical stressors that can trigger the condition, such as:
- Blood loss
- Fever
- Low blood sugar
- Seizure
- Stroke
A notable and unfortunate risk factor is sex. Women, especially middle-aged and post-menopausal women, account for around 90% of cases.
Meet Our Brokenhearted Example
Let’s put a face to broken heart syndrome sufferers. Meet Sloane, a fictional middle-aged woman who has just received a gut-wrenching text message: Her one-and-only has broken up with her, ending their relationship with a sad-face emoji.
Experiencing heartache, Sloane’s body releases a flood of stress hormones. Adrenaline overwhelms her circulatory system, constricting the small arteries that supply blood to her heart.
Her hand goes to her chest as she begins experiencing all the telltale signs: chest pain, shortness of breath, sweating and dizziness. She brushes it off, preoccupied with losing the love of her life, with whom she shared an irreplaceable love of Thai food, horror movies and a popular local indie band whose name escapes her.
As the minutes pass and her symptoms worsen, Sloane realizes the danger she’s in. She dials 911 and makes it to the ER, where testing rules out a heart attack. With follow-up care, including medications for heart muscle weakness, she’s on track to recover fully in a few months, so long as she avoids any more surprises. Lucky for Sloane, most sufferers (95%) never experience another episode of broken heart syndrome.
Don’t Be Afraid to Wear Your Heart on Your Sleeve
Broken heart syndrome is relatively uncommon. Only about 2% of people who seek treatment for a suspected heart attack are diagnosed with the condition. Still, you can always take steps to reduce and manage stress in your life. Exercising, practicing mindfulness and — if you’re experiencing grief — connecting with others in support groups are all great options.
And if you ever go through a breakup, treat yourself to some ice cream, a long walk and the romantic comedy “500 Days of Summer.” Trust us, your heart will thank you.
Ready for More?
We hope we haven’t left you feeling brokenhearted. Medicine is a world brimming with mysteries like broken heart syndrome, waiting for you to explore. And if you’re interested in taking your studies of the human body further, it might be time to consider a career in medicine.
Study Medical Physiology at the University of Florida
At the University of Florida, we offer numerous online medical physiology graduate programs ideal for aspiring medical professionals, including master’s degrees in:
There’s also our online graduate certificate programs, each of which can be completed in as little as one semester. And like our master’s degree programs, our graduate certificate programs are flexible and entirely online, allowing you to study at your own pace and around your schedule.
Whether you’re hoping to fast-track your career in healthcare, education or another field, we’ve got an online program for you. Take a look at our programs, and when you’re ready to take the next step, apply to UF.
Sources:
https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/is-broken-heart-syndrome-real
https://www.mayoclinic.org/diseases-conditions/broken-heart-syndrome/symptoms-causes/syc-20354617#:~:text=People%20with%20broken%20heart%20syndrome,the%20heart%20contracts%20more%20forcefully.
Immunophysiology: How Does the Immune System Work Against Pathogens?
Have you ever found yourself in the middle of cold and flu season, doing everything you can to dodge germs? Or perhaps during summer, you’re wondering if those extra sneezes are seasonal allergies or something more serious. No matter the time of year, understanding how your body defends itself against illness can feel like unlocking the secret to better health.
So, how does the immune system work against illnesses? Specifically, how does it defend against pathogens: the culprits behind illnesses like the flu and the common cold? In this article, we’ll dive into the fascinating field of immunophysiology to explore how the immune system detects, responds to and remembers these harmful invaders.
How Does Your Immune System Work?
The immune system works like a well-honed army, protecting your body against harmful pathogens such as viruses, bacteria, fungi and parasites. This intricate system incorporates specialized cells, proteins and organs that work together to detect and eliminate invaders, while also maintaining a memory of past infections for future protection.
Below, we shine a microscope on the key components of the immune system and their roles:
- Antibodies
These proteins in the blood play a vital role in detecting pathogens. As they circulate, antibodies bind to specific molecules called antigens found on the surface of pathogens. This binding neutralizes the pathogens and marks them for destruction by other immune cells.
- Lymphatic system
Composed of lymph nodes, lymph vessels and lymphocytes (a type of white blood cell), the lymphatic system acts as a transportation network that circulates lymph, a clear fluid containing immune cells, through the body. These lymphocytes seek out and destroy pathogens, aiding in immune defense.
- Spleen
The spleen serves two primary functions: filtering blood and facilitating immune responses. By removing old or damaged red blood cells and pathogens from the bloodstream, it prevents infections from spreading. The spleen also serves as a “surveillance hub,” where immune cells like macrophages and lymphocytes detect pathogens, consume them and activate immune responses.
- Bone marrow
The foundation of the immune system, bone marrow creates the cellular army necessary to fight off pathogens. Located inside your bones, bone marrow is a spongy tissue responsible for producing all blood cells, including white blood cells, which are the star players in your body’s immune defense.
- White blood cells
White blood cells are among the immune system’s most powerful soldiers. They identify and neutralize pathogens, preventing infection. Key types of white blood cells include macrophages, neutrophils and lymphocytes such as T cells and B cells.
- Thymus
This organ functions as a “training ground” for T cells, teaching them to distinguish between the body’s own cells and foreign invaders. This process prevents autoimmune disorders, which occur when the immune system mistakenly attacks the body.
How Is the Immune System Activated?
The immune system activates when it detects pathogens invading the body. This response relies on two types of immunity: adaptive and innate immunity, each playing distinct roles in combating the spread of bacteria or viruses.
But how do these systems work, and what sets them apart? Below, we dive into their mechanisms and the unique contributions they make to immune defense.
Innate immunity
One of the body’s three lines of defense against pathogens, innate immunity is non-specific, meaning it doesn’t target specific pathogens but instead responds to general signs of infection or danger. This system is designed to act quickly, responding to broad features of pathogens, such as their cell walls or other molecular patterns.
Before internal mechanisms of the innate immune system activate, the body has external defenses like the skin, which acts as a physical barrier preventing pathogens from entering the body. In addition to the skin, other barriers like mucus membranes, tears and saliva help block pathogen entry.
If pathogens manage to breach these external defenses — such as through cuts or abrasions — white blood cells like macrophages and neutrophils are the first responders. These cells release cytokines, signaling molecules that initiate inflammation and recruit more immune cells to the infection site. This rapid response is key in controlling infections before the more specific, adaptive immune response takes over.
Adaptive immunity
If the innate immune system doesn’t successfully neutralize a virus, bacterium or other pathogen, the adaptive immune system steps in. This specialized defense system relies on T cells, B cells and antibodies to identify and eliminate specific pathogens. Unlike innate immunity, which is generalized, adaptive immunity can target pathogens with precision, learning from each encounter to respond more effectively in the future.
A hallmark of adaptive immunity is its ability to create immunological memory. When a pathogen invades, T cells and B cells are activated to recognize and destroy it. After the infection is cleared, some T cells (known as memory T cells) remain in the body, primed to recognize the same pathogen if it reappears. Similarly, B cells generate antibodies tailored to the invader, and memory B cells ensure faster antibody production upon reinfection.
This memory mechanism explains why you typically contract certain illnesses, like chickenpox, only once in your lifetime. After your first exposure, your body develops immunity, allowing it to detect and neutralize the pathogen almost immediately during subsequent encounters. Vaccines work on the same principle, training your immune system to recognize specific pathogens without causing illness.
Transform Your Curiosity Into a Career at the University of Florida
Understanding the immune system’s intricate defense mechanisms is fascinating, but it’s just one piece of a much larger puzzle in the field of human health. For those intrigued by topics like immunophysiology, pursuing an advanced degree can deepen your knowledge and open doors to impactful careers in healthcare, research or education.
At the University of Florida, you can choose from numerous online graduate programs in medical sciences, each catering to a unique aspect of anatomy, physiology, pharmacology, anatomical sciences education and so much more.
All of our programs are entirely online, offer multiple start dates each year and can help you achieve your ultimate professional goals in as little as one year. Explore our programs to determine which best aligns with your path, and contact us with any questions you have before applying.
Sources:
https://www.genome.gov/genetics-glossary/Antibody
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/white-blood-cell
https://my.clevelandclinic.org/health/body/24630-t-cells
https://distance.physiology.med.ufl.edu/exploring-the-immune-system-line-of-defense-3-key-strategies/
https://www.niaid.nih.gov/research/immune-system-overview/
Sex-Based Differences in Medicine
Let’s clear up a common myth: men aren’t actually from Mars, and women aren’t really from Venus. While both sexes do hail from the same planet, they also have distinct anatomical and physiological differences. For example, men tend to have thicker skin on their bodies, while women often have greater muscle endurance during exercise because of their body fat percentage and muscle fiber composition.
In medicine, understanding these sex-based differences is critical. A deep knowledge of how anatomy and physiology vary between sexes can impact medical outcomes, treatment effectiveness and even how diseases progress.
The general overview presented here discusses biological sex differences as traditionally categorized in medical literature and may not apply to all individuals, including those who are intersex, transgender or non-binary. We encourage readers to consult with healthcare providers for personalized medical advice.
Male and Female Anatomical Differences
While men and women are metaphorically “cut from the same cloth,” their bodies are not exact replicas. From tissues to bones, distinct anatomical differences are crucial in medical care.
Variations in bone density and muscle composition, for instance, can impact disease susceptibility, surgical approaches and healing times. Recognizing these structural differences allows physicians to tailor treatment plans effectively to each patient’s needs:
- Skeletal structure
Men generally have greater bone density due to higher testosterone levels, while women face a higher risk of osteoporosis, especially post-menopause. This is because estrogen, which helps protect bone strength, declines significantly after menopause, leaving bones more susceptible to weakening.
- Muscle composition
Women tend to have a higher fat-to-muscle ratio, whereas men naturally possess more lean muscle mass. This difference arises from the hormones testosterone and estrogen. Higher estrogen levels in women contribute to body fat storage, while testosterone in men promotes protein synthesis, fostering muscle growth and repair. These hormonal and musculoskeletal distinctions can affect training, physical therapy efforts and recovery times.
- Reproductive anatomy
It’s well known that one of the most significant anatomical distinctions between men and women lies in their reproductive organs. These organs not only play an essential role in procreation but also influence each sex’s vulnerability to specific health conditions. For instance, women are at risk for cervical cancer, while men are prone to complications of the prostate gland. Additionally, pregnancy and childbirth can have lasting impacts on a woman’s health. Physically, these experiences can alter bone density and pelvic structure, and female mental health may be affected by hormonal changes during the (often emotional) transition to motherhood.
Physiological Differences Between Men and Women
Sex-specific physiology also impacts how our bodies respond to illnesses, injuries and treatment plans. Here’s how some of these differences play out across bodily systems:
Cardiovascular system
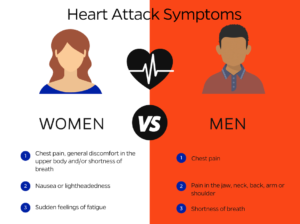
Women generally have smaller hearts and coronary arteries than men, which can affect responses to cardiovascular disease and treatment. For example, men may experience chest pain and arm discomfort during a heart attack, while women often have subtler symptoms, like nausea and shortness of breath.
Respiratory system
Men typically have larger lung volumes, which enhances their oxygen intake and can positively impact their physical endurance. In contrast, women’s smaller lung capacity requires faster breaths during exercise. (But don’t worry, women often excel in endurance events due to their higher proportion of slow-twitch muscle fibers, which contribute to their stamina.)
Additionally, women are more prone to asthma and other respiratory disorders, partly due to higher estrogen levels. Hormonal fluctuations during menstruation and pregnancy can worsen asthma symptoms, suggesting a possible link between hormone levels and respiratory health.
Metabolism
Hormones play a critical role in how our bodies function. Testosterone, in particular, affects metabolism differently in men and women. Because women produce less testosterone, they generally have a lower basal metabolic rate (BMR) than men, meaning they burn calories more slowly and require fewer calories for daily activities.
In addition, women often metabolize certain medications slower than men due to differences in liver enzyme activity. For example, men metabolize the active ingredients in Ambien twice as quickly as women. When physicians first began prescribing this medication, they did not account for this difference in dosage, which led to some adverse effects in women, such as increased drowsiness and impaired cognitive function. This further illustrates why understanding these subtle yet crucial differences in anatomy and physiology is essential for physicians to provide effective care tailored to each sex.
Discovering Your Path in Medicine Begins at UF
Are you interested in leveling up your current role in healthcare? Perhaps you envision yourself as a physician assistant, nurse care manager or distinguished researcher. Whatever the dream, many roles start with a solid foundation in medical sciences.
At the University of Florida, we proudly offer numerous online graduate programs tailored to your diverse interests and aspirations. Whether you’re looking to deepen your knowledge with a comprehensive program in Medical Physiology and Pharmacology or take a specialized refresher in Medical Human Anatomy, our courses provide a convenient, fully online option. This flexibility allows you to continue working in your current role while enhancing the skills that will strengthen your medical school application and improve your clinical expertise.
Explore our robust program selection, which includes both master’s degrees and graduate certificates, to find the path that aligns with your career objectives. Have questions? Don’t hesitate to reach out: We’re here to help you navigate your options and find the best fit for your professional journey.
Sources:
https://www.bbc.com/news/world-49284389
https://weillcornell.org/news/what-women-should-know-about-osteoporosis-and-menopause
https://www.jacionline.org/article/S0091-6749(21)00364-X/fulltext
https://pmc.ncbi.nlm.nih.gov/articles/PMC4773634/
Heart Attack Symptoms in Men vs. Women
According to the Centers for Disease Control, a heart attack occurs every 40 seconds in the United States: roughly the time it takes to send a text or drink a glass of water. Surprisingly, one in five people don’t feel any symptoms, even as damage occurs.
So, how can you recognize if you’re having a heart attack? While sudden chest pain or left-arm pain is often associated with heart attacks, especially for men, symptoms can vary widely by biological sex. Many women experience different, less recognized signs. Knowing the symptoms specific to your sex can make a life-saving difference.
Heart Attacks: The Basics
While heart attacks can appear sudden or out of the blue, they often occur in people with underlying heart disease: a broad term that covers various conditions impacting heart health. Common types of heart disease include:
- Coronary artery disease
- Arrhythmias
- Congenital heart defects
- Heart valve disease
While congenital heart defects are present from birth, other heart conditions typically develop over time, often due to lifestyle factors. In addition, people with heart disease are more likely to experience a heart attack than those without.
A heart attack occurs when blood flow to the heart is blocked, stopping circulation and oxygen to heart tissue. The longer the delay in restoring blood flow, the greater the potential damage to the heart muscle. Early treatment is crucial to minimize harm and improve recovery outcomes, which is why it’s so important to understand the symptoms you may experience depending on your sex.
Why Are Women’s Heart Attack Symptoms Different From Men’s?
There are several potential reasons why women might not always experience the same symptoms as men during a heart attack:
- Biological differences
Women often have smaller hearts and blood vessels than men, which affects how heart disease develops. This difference can lead to more blockages in the smaller coronary arteries, resulting in atypical symptoms like shortness of breath, fatigue and jaw or back pain rather than the intense chest pain commonly seen in men.
- Hormonal differences
Before menopause, estrogen can provide a protective effect on women’s hearts. After menopause, when estrogen levels decrease, women’s heart disease risk rises sharply. This shift can contribute to the onset of different heart attack symptoms.
Common Heart Attack Symptoms in Women
While chest pain is still the leading symptom of heart attacks in women (as well as men), there are other signs to look for. Recognizing these signs can make a critical difference, leading to faster treatment and potentially saving heart muscle in the process.
Here are some other common women’s heart attack symptoms:
- Sudden dizziness.
- Heartburn-like discomfort that may be mistaken for acid reflux.
- Unusual fatigue without a clear reason.
- Nausea or vomiting, especially when accompanied by other symptoms.
- Pain in the upper body, including one or both arms, the back, neck, jaw or stomach.
Symptoms of a Heart Attack in Men
For men, some of the most common symptoms of a heart attack include:
- Chest pain: This often feels like a sudden pressure, squeezing or tightness in the left or center of the chest.
- Shortness of breath: This symptom is more common in older adults and can occur before or while experiencing chest pain.
- Pain in the upper body: Men often experience discomfort in the arms, jaw, stomach, neck or back during a heart attack.
Become a Leader in Cardiovascular Health
Recognizing the differences in men and women’s heart attack symptoms is essential to acting quickly if you or someone you know experiences signs of a heart attack. If you’re captivated by the cardiovascular system and passionate about helping others prevent and manage heart disease, have you considered a career in medicine?
Whether you aim to become a physician, researcher or another healthcare professional, the University of Florida can help you take the next step. Our online Graduate Certificate in Medical Physiology with a Specialization in Cardiovascular/Renal Physiology is a 12-credit program that offers a comprehensive foundation in five key body systems, with a special focus on areas like hypertension and blood circulation. For a broader skill set, explore our other graduate degrees and certificates tailored to meet your interests and career goals.
All programs are entirely online and ideal for working professionals seeking career advancement while maintaining a balanced work-life schedule. Plus, with competitive tuition and year-round start dates, we’re ready to welcome you whenever you’re ready to begin your next chapter.
Sources:
https://www.cdc.gov/heart-disease/data-research/facts-stats/index.html
https://www.mayoclinic.org/diseases-conditions/heart-disease/symptoms-causes/syc-20353118
https://give.brighamandwomens.org/7-differences-between-men-and-women/
How Does Exercise Affect Your Body?
It’s easy to push exercise to the bottom of your to-do list. You might catch yourself saying, “I’m too tired,” or “I’ll do it tomorrow” time and again. But have you ever stopped to think about the real benefits of incorporating regular physical activity into your life?
You’ve probably heard a lot from those around you: “You’ll sleep better,” “I lost 20 pounds,” or “You’ll feel amazing!” But what do those things truly mean? How does exercise affect your body?
The reality is that you don’t need to stick to just one type of workout to experience the benefits. From cardio to strength training, all forms of physical activity have both short- and long-term benefits. Who knows? Learning how your body responds to exercise might be just the motivation you need to say, “Today’s the day.”
Cardiovascular System
Your cardiovascular system is responsible for delivering oxygen and nutrients to your muscles and organs while removing waste products like carbon dioxide. Without putting it under some much-deserved exercise-related stress, it’s more likely to weaken over time, increasing the risk of cardiovascular diseases. Even a 15-minute walk is enough to get your blood pumping and kick your cardiovascular system into high gear, keeping it strong and efficient.
- Short-term effects
Whether you go for a brisk walk or swim laps at the community pool, any exercise will cause an immediate rise in your heart rate. This happens because your muscles need more oxygen to produce energy. In response, your heart works harder, pumping oxygen-rich blood to fuel your muscles. (This is why your muscles may appear and feel fuller during and right after exercise: they’re temporarily filled with extra blood.)
- Long-term effects
Making exercise a regular part of your routine — whether through cardio or strength training — can lead to improved blood pressure regulation over time. This is particularly beneficial for individuals who are prone to high blood pressure, as consistent physical activity can help lower and maintain healthy blood pressure levels.
Musculoskeletal System
When you engage in exercise, your bones, joints and connective tissues undergo several important changes:
- Short-term effects
After a few sets of dumbbells, you may experience a temporary boost in strength and power. This is due to the activation of your muscle fibers, which respond to the demands placed on them. A day or two post-exercise, you might notice soreness in the muscle groups you targeted. This sensation arises from microscopic tears in your muscle fibers — a natural part of the process. If your goal is to tone your muscles or build mass, this soreness is a positive sign, as it indicates that your muscles are on the path to growth through continued tearing and healing.
- Long-term effects
Muscle hypertrophy, or growth, doesn’t occur overnight. It requires consistent strength training, gradually increasing both your repetitions and weights over time. Alongside muscle growth, you can also expect improvements in coordination and flexibility. These benefits are partly due to the increased bone density that comes with regular exercise, contributing to a healthier and stronger musculoskeletal system.
Respiratory System
Whether you’re perfecting a new yoga pose or training for your first half marathon, breathing is a fundamental component of exercise. It enables your body to receive the oxygen it needs to perform at its best. Here’s what happens to your respiratory system when you engage in exercise:
- Short-term effects
During your workout, you’ll notice an increased breathing rate, which means you’ll begin to breathe more quickly. This boost enhances your oxygen uptake because your body requires more oxygen to fuel your muscles.
- Long-term effects
After a few repeat workouts, you’ll experience improved lung capacity, strengthening not just your muscles but also your lungs. One of the most significant benefits of consistent exercise on your respiratory system is improved endurance. For instance, when you begin your exercise journey, you might only be able to jog comfortably for five minutes before feeling out of breath. However, with weeks of consistent effort, you’ll find that your endurance has improved, allowing you to jog for twice as long without feeling winded.
Metabolic Changes
What about weight loss? In both the short and long term, exercise offers several metabolic benefits that impact calorie burn and weight management:
- Short-term effects
During exercise, your body burns significantly more calories compared to when you’re at rest. This is due to the increased energy demand placed on your muscles. If one of your goals is to lose weight, you’ll need to create a calorie deficit, meaning you burn more calories than you consume. By exercising regularly, while maintaining a balanced diet, you’re more likely to shed excess weight as a natural outcome of this energy expenditure.
- Long-term effects
Over time, exercise helps build muscle mass, which elevates your resting metabolic rate. This means you’ll continue burning more calories even when you’re not actively working out, creating a cycle that supports both muscle maintenance and weight management. It’s a win-win for your metabolism and overall health!
Find Your Niche in Healthcare at the University of Florida
Understanding how exercise affects your body at the physiological level not only helps you achieve personal fitness goals but also opens doors to broader applications in healthcare. If you’re passionate about these topics and want to deepen your knowledge, the University of Florida offers online graduate programs in the medical sciences. Whether you’re interested in clinical research, personal training or physical therapy, UF’s programs equip you with the skills to make a meaningful impact in the health industry.
From an online master’s degree in medical physiology and pharmacology to an online Graduate Certificate in Medical Human Anatomy (and so many more), there are numerous paths to choose from, depending on your interests and what roles you picture yourself in.
Explore all of our entirely online program options to choose the program that best aligns with your professional goals.
Sources:
https://www.health.harvard.edu/heart-health/the-many-ways-exercise-helps-your-heart
https://www.nsca.com/contentassets/d27e2ba7e56949229d3eb1aaef7ddcfa/trainertips_hypertrophy_201601.pdf?srsltid=AfmBOorWvSuKwwXKmF_KE55YGh0bF3La2gE08_3i82_QieoVxOtwZOOR
https://orthoinfo.aaos.org/en/staying-healthy/exercise-and-bone-health/
https://pubmed.ncbi.nlm.nih.gov/27348753/
What Are the Impacts of Stress on the Body and Mind?
It’s late afternoon, and you have an hour’s worth of work piled on your desk with a tight deadline looming. Yet, you have to leave in 30 minutes to pick up your children from school. The clock is ticking, and the stress is mounting.
Our stress response, commonly referred to as the “fight-or-flight” reaction, can be triggered by everyday challenges such as work pressures, financial worries, traffic congestion and family obligations. But how do these stressors affect our bodies and mental health?
In this article, we will explore three types of stress and examine how prolonged exposure to stress can impact you mentally and physically.
Types of Stress
There are three main types of stress that a person experiences:
- Acute stress
This is short-term stress that everyone faces from time to time. It typically arises from temporary challenges, like meeting a deadline or having an argument. Acute stress can cause physical reactions, such as a racing heart or sweaty palms.
- Episodic stress
When acute stress becomes frequent, it can make it harder to return to a relaxed state. People who tend to overcommit or worry constantly often experience episodic acute stress. The effects are similar to acute stress but can also include irritability, anxiety and digestive issues.
- Chronic stress
Chronic stress occurs when someone feels stressed for weeks — or even longer. It is often triggered by ongoing challenges like financial problems, work issues or relationship struggles. This type of stress is the most harmful because it causes prolonged elevation of the stress hormone cortisol, which can increase the risk of serious health problems over time.
Physical Impacts of Stress
The physiological impacts of stress are extensive and affect several areas of your body. Below, we discuss some of the common impacts that stress causes in each bodily system:
Cardiovascular and Respiratory System
- Increased blood pressure
The release of cortisol can cause your heart to beat faster and narrow your blood vessels, leading to a temporary increase in blood pressure.
- Increased breathing rate
In stressful situations, your breathing often quickens to supply more oxygen to your muscles. For individuals with pre-existing conditions such as asthma or emphysema, this can exacerbate breathing difficulties as stress causes airway constriction.
- Increased risk of heart disease
Chronic stress can keep blood pressure elevated for long periods, significantly raising the risk of developing cardiovascular issues such as heart disease, heart attacks or strokes.
Immune System
When stress persists, the prolonged release of cortisol and other stress hormones can suppress the immune response, leaving you more vulnerable to infections and slowing down your recovery time. Over time, this weakened immune state increases the risk of both acute illnesses and chronic conditions.
Digestive System
Have you ever felt a sudden case of nerves before a big work meeting or job interview? Maybe you experienced butterflies that turned into an impromptu trip to the bathroom. Whatever the trigger, stress can wreak temporary havoc on your digestive system in several ways.
Sometimes stress causes gastrointestinal issues, like irritable bowel syndrome or acid reflux. It may also impact your appetite, causing you overeat or lose your appetite altogether. These effects may stem from the brain-gut connection, a network of nerves that allows the brain and gut to communicate. During periods of stress, the gut may become hypersensitive, leading to discomfort, bloating or other digestive disturbances.
Musculoskeletal System
When you’re stressed, your muscles become tense. During short-term (acute) stress, this tension usually dissipates once the stressor is gone. However, chronic stress can leave your muscles in a constant state of tightness, which may lead to:
- Headaches
- Back pain
- Worsening of musculoskeletal conditions such as fibromyalgia
Impact of Stress on Mental Health
Your mind isn’t the only part of your body affected by short- or long-term stress. Chronic stress can also take a toll on your mental health, causing numerous issues, like:
- Anxiety disorders
- Depression
- General burnout
- Difficulty concentrating
- Low sex drive
Stress Management Techniques
While stress can sometimes feel unavoidable, there are proactive steps you can take to minimize its impact:
- Mindfulness and relaxation techniques
According to a study by the National Institutes of Health, regular meditation practice can help reduce cortisol levels in the body, promoting both mental and physical relaxation. Additionally, deep breathing exercises and yoga are effective methods for counteracting the physiological effects of stress. These practices can enhance emotional well-being and provide tools for managing stress in everyday life.
- Therapy
Counselors and therapists offer various techniques to help patients manage stress, ranging from traditional approaches like cognitive behavioral therapy (CBT) to more contemporary methods such as mindfulness-based stress reduction (MBSR).
- Lifestyle changes
Exercise releases endorphins, which can naturally give you a boost in the mood department. It can also improve your sleep quality, which is essential for reducing stress.
Explore UF’s Graduate Programs in Medical Sciences
Recognizing the impacts of stress on both the body and mind is crucial, especially for those considering a career in the medical field. If you’re interested in deepening your understanding of the physiological responses to stress and how they relate to health outcomes, the University of Florida offers several online graduate credentials in medical sciences to choose from:
- Master’s Degree in Medical Physiology and Pharmacology
- Master’s Degree in Medical Physiology and Aging
- Master’s Degree in Medical Anatomy and Physiology
- Graduate Certificate in Medical Physiology
- Graduate Certificate in Medical Physiology with a specialization in Cardiovascular/Renal Physiology
- Graduate Certificate in Medical Anatomy and Physiology
- Graduate Certificate in Medical Human Anatomy
Explore our course offerings to find the path that aligns with your professional aspirations. When you’re ready, the application — and your future — are just a click away.
Sources:
https://my.clevelandclinic.org/health/diseases/11874-stress
https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress/art-20046037
https://www.apa.org/topics/stress/body
https://my.clevelandclinic.org/health/body/the-gut-brain-connection
https://pubmed.ncbi.nlm.nih.gov/22377965/
How Do Vitamins Work? The Science Behind Their Absorption
Many of the foods we eat naturally contain vitamins and other nutrients, while others are fortified, such as milk with added vitamin D. Still, some people lack certain essential vitamins due to their diet, age, gender, genetics or other factors. To compensate, many take supplements, such as multivitamins, that deliver a variety of vitamins and minerals in every dose.
How do vitamins work in the body? Let’s explore this topic and examine the ongoing controversy surrounding supplement efficacy within medical and scientific communities.
How Do Vitamin Supplements Travel Through Your Body?
Here’s a step-by-step explanation of how vitamins travel through the human body:
- You swallow the vitamin supplement, and it moves down the esophagus to the stomach.
- In the stomach, digestion begins. Digestive acids and enzymes begin to dissolve the supplement, but it’s not fully digested here.
- The remaining portion travels to the small intestine, where it’s further broken down by digestive enzymes and fluids from the liver and pancreas.
- In the second and third parts of the small intestine, nutrients from the digested supplement are absorbed into the intestinal lining. From here, the method of entry into the bloodstream depends on the type of vitamin:
- Water-soluble vitamins (B and C) are absorbed directly into the bloodstream.
- Fat-soluble vitamins (A, D, E and K) must be broken down by bile acids before being absorbed. These are then absorbed by the lymphatic system and transported into the bloodstream.
- The bloodstream carries the beneficial portions of the vitamin to various cells and tissues in the body.
- Excess water-soluble vitamins and their byproducts exit the body through urine, while remaining fat-soluble vitamins are stored in the liver and fatty tissues for later use.
What Is the Role of Vitamins in Our Bodies?
Vitamins play crucial roles throughout the body, aiding each organ, tissue and cell in different ways. They help:
- Fight infections
- Improve vision
- Build strong bones and muscles
- Regulate hormones
Many cells in our bodies, from skin to bone, regenerate regularly to replace old and damaged ones. For example, the outer layer of our skin cells renews about once a month. This regeneration process requires vitamins, whether obtained from food or supplements, making them essential to the normal, healthy functioning of the body.
What’s the Controversy Behind Vitamin Supplements?
While taking vitamin supplements may seem beneficial, many experts argue that vitamins in supplement form provide little to no health value compared to those obtained through food. Some point to scant evidence that supplements prevent or cure any major diseases.
Others contend that the body does absorb beneficial vitamins from supplements but eliminates excess amounts through urination — a potentially favorable scenario. Most experts agree that the best way to obtain vitamins is through a nutrient-rich diet rather than supplements.
Fortify Your Career with a Master of Science from UF
Vitamins, drugs and other compounds can profoundly impact the major human body systems. We examine their beneficial and detrimental effects in the University of Florida’s online Master of Science in Medical Sciences with a concentration in Medical Physiology and Pharmacology, offered through our College of Medicine.
Built around an MCAT-aligned curriculum, our 30-credit MS program prepares you for medical school or nursing school admission and a variety of rewarding careers in medicine, science, pharmacy and research.
- Earn your master’s degree entirely online — no campus or lab visits required.
- Get started with no GRE requirement.
- Complete coursework at your own pace from practically any location.
- Maintain your professional commitments.
- Transfer up to 15 credits from a qualifying UF graduate certificate program.
- Finish your degree in as little as two semesters.
Add a respected master’s degree to your career credentials. Apply today!
Sources:
https://ods.od.nih.gov/factsheets/WYNTK-Consumer/
https://www.hopkinsmedicine.org/health/wellness-and-prevention/is-there-really-any-benefit-to-multivitamins
https://www.prevention.com/life/a20474960/how-to-make-sure-youre-benefiting-from-your-vitamins/
https://health.clevelandclinic.org/which-vitamins-should-you-take
https://my.clevelandclinic.org/health/body/7041-digestive-system
https://time.com/6171584/are-vitamins-supplements-healthy/
Drugs That Treat Multiple Conditions: Hydroxyzine
Throughout the pharmaceutical world, there are numerous drugs that help people manage multiple conditions. Topiramate, developed to treat seizures, doubles as a migraine treatment. Bupropion, typically prescribed as an antidepressant, also aids in smoking cessation. Minoxidil, developed to treat high blood pressure, is perhaps better known for reversing hair loss.
Clinical trials determine the effectiveness and safety of drugs before they’re approved for public use, but sometimes these trials reveal unforeseen benefits. Hydroxyzine is a prominent example of this type of versatile medication, and one we’ll explore its multiple uses in this article.
Hydroxyzine: A Versatile Medication
Hydroxyzine, a prescription antihistamine typically administered orally, has applications beyond stopping runny noses. As an antihistamine, hydroxyzine is commonly used as a treatment for allergies and allergic reactions, such as certain types of eczema, dermatitis, hay fever, asthma and conjunctivitis. Its additional uses include:
- Anxiety treatment
- Sedation before medical procedures
- Nausea and vomiting relief
- Motion sickness symptom alleviation
Some studies, including those conducted by UF Health, also suggest that the anti-inflammatory response of hydroxyzine lowers the risk of death among hospitalized COVID-19 patients.
How Hydroxyzine Works
Hydroxyzine, an H1-blocker, impedes the effects of histamine, a chemical produced within the human immune system. It crosses the blood-brain barrier and interacts with serotonin and dopamine receptors, producing sedative and anxiety-reducing effects.
H1-blockers such as hydroxyzine stop histamines from binding to histamine receptors, which can be found throughout the body, including on glandular and mast cells, smooth muscle, and nerves. Histamines widen blood vessels and make them more permeable, leading to fluid leakage from capillaries into adjacent tissues. H1-blockers prevent these actions, effectively reducing inflammation and alleviating allergy symptoms.
If an inflammatory condition leads to chronic inflammation, treatment is essential for the prevention of damage to organs and DNA and the development of several serious diseases, including cancer and heart disease.
Master Drug Mechanisms and Advance Your Medical Sciences Career
The University of Florida’s online Master of Science in Medical Sciences with a concentration in Medical Physiology and Pharmacology explores how various drugs and substances affect body systems and overall human health. Our 30-credit program enables you to gain crucial knowledge and a valued credential that can lead to a rewarding career as a:
- Physician
- Physician assistant
- Nurse
- Clinical scientist
- Professor
- Researcher
Our program’s MCAT-aligned curriculum helps prepare you for admission to medical school or nursing school and can distinguish you among a wide field of candidates in a highly competitive admissions environment where about 60% of medical school applicants are rejected annually.
Benefits of Online Learning
As an online student, you’ll complete your degree entirely online. No campus or lab visits are required. This empowers you to:
- Access coursework from practically anywhere.
- Work at your own pace.
- Connect with classmates and faculty anytime through email, discussion groups and other online tools.
- Network with students from the U.S. and around the world for broader career prospects.
- Earn a graduate credential while meeting your professional and personal obligations.
Start Sooner and Finish Faster
Our online master’s degree in medical physiology and pharmacology program does not require GRE scores, enabling you to bypass that common admission step. And you can collect your online master’s degree in medical physiology and pharmacology sooner — in as little as two semesters — if you’ve already completed a qualifying UF graduate certificate program. We allow you to transfer up to 15 credits to this MS program from your:
Choose an Institution Acclaimed for Quality
This master’s degree program is bolstered by UF’s exceptional reputation and accolades:
- Liaison Committee on Medical Education (LCME)-accredited College of Medicine
- Renowned faculty comprised of the same accomplished researchers and physicians who teach UF’s medical students
- Acknowledgements including:
Prime yourself for greater opportunities ahead. Apply now!
Sources:
https://www.mayoclinic.org/drugs-supplements/hydroxyzine-oral-route/description/drg-20311434
https://my.clevelandclinic.org/health/drugs/20775-hydroxyzine-solution
https://my.clevelandclinic.org/health/articles/24854-histamine
https://health.usnews.com/wellness/slideshows/8-medications-that-treat-multiple-conditions?slide=9
https://www.aocd.org/page/antihistamines?
How Does Nicotine Replacement Therapy Relieve Addiction?
”From a scientific standpoint, nicotine is just as hard, or harder, to quit than heroin.” This jarring statement from nicotine researcher Dr. Neil Benowitz may explain why so many people struggle with giving up nicotine for years, or even a lifetime.
When individuals use conventional cigarettes, cigars, chewing tobacco or e-cigarettes, the bloodstream quickly absorbs the chemical nicotine and transports it to the brain. The brain responds by releasing dopamine, the “happy hormone,” producing a pleasurable sensation. The body eventually grows accustomed to that sensation and becomes dependent on nicotine to produce it. When a smoker quits cigarettes, they may begin to feel angrier, sadder and hungrier due to the lack of stimulation from nicotine. They start to crave that happy hormone feeling. This is nicotine addiction.
Viable Alternatives to Nicotine
Overcoming nicotine addiction is no easy task for many. But there are substitutes for nicotine that are designed to wean addicts off of this harmful substance. In 1984, nicotine addicts found a new hope as the Food and Drug Administration (FDA) approved nicotine replacement therapy (NRT). NRT products were first introduced in the form of gum, then later patches, lozenges, inhalers and other methods. Many of these were originally offered by prescription only but subsequently became available over the counter.
NRTs act upon the receptors in the brain that are affected by nicotine, easing the cravings and withdrawal symptoms that most people who give up nicotine experience. Quite often, using multiple NRT methods at the same time yields better results. According to researchers, NRTs boost tobacco quit rates by up to 70%. In most cases, therapy involves gradually reducing the amount of nicotine and/or frequency of the use of NRT until the user is weaned off the addictive chemical altogether.
It should be noted that while many nicotine users are able to overcome their physiological dependence on nicotine through NRT, such products do not alleviate any behavioral associations that tobacco users develop. For example, some smokers associate pleasure with the act of picking up a cigarette and placing it in their mouth or just feeling the sensation of having a cigarette between the lips. For this reason, behavioral therapy is often recommended alongside or following NRT.
Master Physiology and Pharmacology Online
The University of Florida’s renowned College of Medicine provides degree and certificate programs that will help you understand how nicotine and other substances can impact human physiology and broaden your knowledge of body systems overall. Each of these programs is presented entirely online, which allows you to complete a respected education credential on your own schedule, around any professional and personal responsibilities you may have. All programs are available 24/7 from just about any location.
Master of Science in Medical Sciences with a concentration in Medical Physiology and Pharmacology
Our online master’s degree in medical physiology and pharmacology program explores the major human body systems and how different drugs impact and are impacted by them. In addition, our program helps you prepare for National Board, MCAT and other key exams that can enable you to advance into a new role in your medical career. You may be able to finish this program in as little as one year.
What’s more, if you have completed a Graduate Certificate in Medical Physiology or a Graduate Certificate in Medical Physiology with a specialization in Cardiovascular/Renal Physiology (more information below), you’re already halfway to earning a master’s degree in medical physiology and pharmacology. Our 30-credit degree program accepts up to 15 credits from these UF graduate certificate programs. Consider the advantages of our master’s degree in medical physiology and pharmacology program:
- Earn your master’s degree in as little as one year.
- Complete coursework at your own pace.
- Build clinical knowledge that can help you excel in medical school.
- Get started without taking the GRE.
- Use financial aid options, if needed.
- Add a career-defining education credential to your resume.
Graduate Certificate in Medical Physiology
Our Graduate Certificate in Medical Physiology investigates the fundamentals of the field and explores individual systems of the human body. You can take as many as six courses in this 9- to 14-credit program, though you are only required to complete 9 credits. That means you may be able to complete the program in a single semester.
Graduate Certificate in Medical Physiology with a specialization in Cardiovascular/Renal Physiology
We also offer a Graduate Certificate in Medical Physiology with a specialization in Cardiovascular/Renal Physiology, an advanced-level look at cardiovascular and renal physiology and pathophysiology that you’ll find invaluable in a clinical setting. You can complete this 12-credit program in as little as two semesters.
Find out how the human body functions and interacts with different drugs and other substances in an entirely online master’s degree or graduate certificate program from the University of Florida.
Sources:
https://www.psychologytoday.com/us/basics/dopamine
https://www.drugabuse.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/nicotine-addictive
https://www.cancer.org/healthy/stay-away-from-tobacco/guide-quitting-smoking/nicotine-replacement-therapy.html
https://www.verywellmind.com/nicotine-replacement-therapy-4013217
https://www.sciencedaily.com/releases/2016/08/160831085320.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5003586/
https://www.healthline.com/health/oral-fixation#examples-in-adults
Becoming an Astronaut: How Space Flight Affects Our Bodies
As children, many of us shared a similar professional goal: We were determined to become astronauts. Little did we know that NASA’s acceptance rate is abysmally low. In 2024, more than 8,000 people applied to become astronauts. Of that number, NASA will only choose between eight and 12 candidates.
Beyond the rigorous selection process, one aspect of being an astronaut that we likely didn’t consider as children is the effect space flight has on our bodies. With drastic changes in gravity and no atmosphere to shield us from the sun’s UV rays, several short- and long-term changes can occur in our bodies while in space.
Settle in and buckle up as we explore the effects of space flight on humans and — for those still interested — the prerequisites for becoming an astronaut.
Immediate Effects During Launch
In addition to the adrenaline spike they may feel during the famed countdown to liftoff, astronauts may experience several other physiological changes during space shuttle launches due to increased G-forces, including:
- Difficulty moving limbs.
- Tunnel vision or brief loss of consciousness.
- A reduced ability for the heart to efficiently pump blood.
- Bodily fluids shifting upward, which can cause fluid retention in the upper body.
- Discomfort in the sinuses due to changes in air pressure.
Musculoskeletal Adaptations
If you’re on a commercial mission to space, you’ll likely only be there long enough to appreciate the beauty of Earth from above, notice its curvature and maybe even experience a few sunsets or sunrises, depending on your positioning. Astronauts on extended missions will remain in space much longer. The average duration of an astronaut’s mission aboard the International Space Station (ISS) is 6 months.
Half a year is plenty of time for the lack of gravity to take a toll on your musculoskeletal system (i.e., your muscles and bones). On Earth, your body constantly uses its muscles to resist the force of gravity. In space, however, there’s no gravity to fight, so you end up using your muscles significantly less.
Over time, living in a zero-gravity atmosphere can weaken your muscles and reduce bone mass. Fortunately, astronauts can mitigate the effects of these unique conditions before, during and after a mission by engaging in a rigorous exercise routine. During their time on the ISS, astronauts exercise for about two hours a day, strengthening their bodies by using a treadmill and incorporating strength training.
Changes to the Immune System
Having lived on Earth your entire life, your immune system has adapted to function under Earth’s gravitational pull. Experiencing altered gravity in space impairs your immune system’s peak performance. In addition to microgravity, increased radiation and disrupted circadian rhythms can also impact your immune system.
A weakened immune system might result in your body fighting harder and longer to combat an infection it could easily overcome on Earth. You might also become more susceptible to infections until you return to Earth’s normal conditions and your immune system readjusts.
Psychological and Cognitive Effects
Physical changes aren’t the only effects to expect while spending an extended period in space. Being away from family and in constant close quarters with the same small group of people for months can impact your mental well-being, leading to feelings of isolation or confinement.
Astronauts prepare for these psychological effects through several strategies, including:
- Undergoing psychological resilience training before the mission.
- Participating in simulated missions to acclimate to the cognitive demands of space travel.
- Establishing a structured daily routine while in space to maintain normalcy.
- Contacting family regularly via email and video calls.
- Bringing personal items and participating in group activities and hobbies aboard the ISS.
- Having regular check-ins and psychological assessments.
Do You Have What It Takes for a Trip to Space?
While astronauts face several mental and physical hurdles as they embark on expeditions in space, they’re also pioneering scientific research that could change the future of science, technology and the way we live. Although many people believe they have what it takes to become an astronaut, it requires more than just determination. In addition to being a U.S. citizen and having a minimum of three years of related professional experience, you need a master’s degree in a STEM field from an accredited institution.
Whether you aspire to become an astronaut or you’re interested in turning your fascination with the human body into a lucrative career, the University of Florida offers several online graduate programs ideal for those interested in advancing their careers in health and sciences:
Our online programs in medical physiology, offered by one of U.S. News’ top 50 national universities, also boast the following benefits:
- Affordable tuition rates.
- Year-round start dates.
- No GRE requirement.
- Flexible coursework completion on your timeline.
Take the first step in advancing your career in the expansive and profitable world of STEM — apply today!
Sources:
https://touroscholar.touro.edu/cgi/viewcontent.cgi?article=1077&context=sjlcas
https://www.kennedyspacecenter.com/blog/the-20-most-frequently-asked-questions-about-the-international-space-station
https://www.nasa.gov/missions/station/scientists-probe-how-long-term-spaceflight-alters-immunity/
https://www.abc.net.au/news/health/2024-03-09/preparing-human-mind-space-travel-mars-astronauts-mission/103563280



