Category: Physiology
Biotechnology in Cardiovascular Care: How Targeted Drug Delivery Is Saving Lives
Every 1.5 seconds, someone dies of cardiovascular disease. It’s the world’s leading killer, responsible for 38% of premature deaths under 70 and 19.8 million lives lost in 2022. Those aren’t just numbers — they’re parents, siblings and friends.
Now, imagine you walk into a hospital bracing for bad news, only to hear your cardiologist say, “We’ll just grow you a new blood vessel. Maybe even an entire heart.” Thanks to biotechnology, this will soon sound less like science fiction. Let’s look at how biotechnology advances are transforming heart care and saving lives.
What Is Targeted Therapy for Heart Care?
Imagine you could fix a broken heart by simply mending it, one piece at a time.
It’s like patching a leaky pipe in a building: You don’t demolish the whole thing right away, right? You try to fix the problem exactly where it is first. This is how targeted therapy for cardiovascular conditions works, too.
Right now, scientists can:
- Grow heart tissue in a lab to patch damaged areas
- Edit faulty genes that cause disease
- Send medicine directly to the part of the heart that needs it (while leaving healthy parts alone)
Getting Medicine to the Right Place
Here’s the tricky part: It’s not just about what to treat the heart with, but how to get it exactly where it’s needed. Some of the strategies scientists are exploring are:
- Passive targeting
This strategy lets the body guide the medicine. Damaged heart tissue absorbs tiny drug particles, allowing drugs to target only the areas that need them.
- Active targeting
Now imagine drugs outfitted with tiny “GPS navigators” (yes, really) so they lock only onto sick cells and skip the healthy ones.
- Smart release
These designer drug carriers only open when they sense certain changes — for example, acidity after a heart attack — or, when triggered by something outside the body, like a magnet or ultrasound.
Now that we understand the basic approaches, let’s explore how scientists are putting these ideas to work with some of the most promising treatments in development.
Nanoparticles: Undercover Medical Helpers
Nanoparticles are ultra-tiny carriers that can slip past the body’s defenses. They sometimes wear a disguise so the immune system waves them through, delivering drugs precisely where they’re needed.
Scientists are already leveraging nanoparticle technology. One group of researchers developed a prototype that targets the heart after an attack, releasing anti-inflammatory medicine only where the heart needs it. Another type of nanoparticle drug can be inhaled. Imagine fixing a heart problem with something as simple as an inhaler instead of needing surgery. It would make battling heart conditions a lot less stressful and life-changing!
mRNA and Gene Editing: Rewriting the Code
Some cardiovascular issues are hereditary, like cardiomyopathy (which is the leading cause of heart failure). In these cases, the only real fix may be to cut faulty genes out entirely.
CRISPR is a tool that can cut specific genes from a DNA strand. In one trial, a single CRISPR treatment lowered harmful cholesterolrelated proteins by more than 90%. This is an example of the type of “one-and-done” cure scientists are looking for.
The Biological Bypass: Growing New Blood Vessels
What if parts of the heart aren’t getting enough blood? One option is to grow new blood vessels to replace the damaged ones.
Biodegradable scaffolds seeded with a patient’s own cells, for example, can become living tissue. Another approach, therapeutic angiogenesis, uses gene therapy or special proteins to stimulate vessel growth. It’s like bypass surgery … performed by your own body.
Precision Treatment and Designer Drugs
Heart medications are often prescribed to treat the disease and not the person. These medications, like beta blockers, affect the entire body. Targeted delivery makes treatment much more precise.
Here are some precision treatment methods currently changing medicine as we know it:
- Afterloadreducing drugs
Common medicines like ACE inhibitors (prescribed for individuals with enlarged hearts) could be paired with delivery systems that act mainly on the heart and blood vessels, easing strain without affecting other tissues.
- Inclisiran
This RNAbased treatment turns off a specific gene causing heart conditions.
- Nanovesicles
These tiny carriers are used to carry drugs, genetic material, or regenerative factors directly to damaged heart muscle.
The Future of Cardiovascular Care: What We’ve Learned
Can you imagine a heart patch made from your own tissue that only releases drugs when there’s a problem? We may not be too far from this reality.
Here’s what’s been changing in cardiovascular care:
- Precision targeting is delivering medicine straight to damaged heart tissue.
- Smart tech like CRISPR, mRNA and nanoparticles are making treatments more precise.
- Pills aren’t the only answer: New drug carriers like nanovesicles can deliver regenerative compounds or gene therapy.
The future of heart care is personalized: designed for your unique biology.
Study the Science That’s Redefining How We Heal the Heart
If breakthroughs like lab-grown heart tissue and gene editing excite you, imagine being part of the team making them possible. At the University of Florida, researchers are pushing boundaries in targeted cardiovascular drug delivery, including physiology-guided nanotherapeutics.
UF’s entirely online medical sciences programs can help you build the necessary foundation to turn your curiosity into a career, whether it leads to biotechnology, physiology, pharmacology or a combination of all these. You’ll choose from a range of graduate options like Medical Physiology and Pharmacology or stack skills with a Medical Physiology Graduate Certificate.
These programs give you a deep understanding of how the heart and body work, and how to design treatments that are precise and effective, preparing you to join the future of heart care and the people that will build it.
Because one day soon, “We’ll grow you a new heart” won’t make headlines. It’ll just be everyday healthcare.
Sources:
https://www.sciencedirect.com/science/article/pii/S2666667724000692
https://pubmed.ncbi.nlm.nih.gov/33500578
7 Surprising Effects of Sugar on the Body
If you enjoy a sweet treat after dinner (or even lunch — we don’t judge), you’re in good company. In one study, 61% of U.S. adults reported finding their own little moment of happiness in something sweet on any given day. Whether your favorite treat is gummies, chocolate, ice cream or cookies, chances are it’s packed with sugar.
Having the occasional sugar-filled indulgence is fine. You only live once, after all.
But did you know that adult men consume an average of 24 teaspoons of added sugar each day? If they’re only having one little dessert a day, where is all that sugar coming from?
Common Sources of Added Sugar
You’re probably consuming more sugar than you realize, and it’s sneaking in through everyday foods and beverages. That tablespoon of ketchup with your fries? A small but significant 3 grams of sugar. A half-cup of your favorite fat-free flavored yogurt? Around 12 grams. And that afternoon can of Coke? A whopping 39 grams.
So, what does all this hidden sugar do to your body? Excess sugar can disrupt metabolism, promote fat storage, increase inflammation, and impact your energy levels.
Here are seven surprising ways sugar affects your body, from quick energy spikes to long-term health risks.
7 Ways Sugar Impacts Your Body
#1 Leads to Insulin Resistance
When you frequently consume foods and drinks with added sugar, especially sweetened beverages, your blood sugar spikes, prompting your body to release more insulin. Over time, this can lead to insulin resistance, where your cells stop responding properly to insulin. It’s a major early warning sign for type 2 diabetes.
#2 Contributes to Fatty Liver Disease (NAFLD)
Our bodies break down fructose (an essential ingredient in table sugar and high-fructose corn syrup) in the liver. When consumed in excess, it can cause fat buildup in liver cells, leading to non-alcoholic fatty liver disease (NAFLD).
Over time, NAFLD can contribute to:
- Liver inflammation
- Scarring
- Long-term liver damage
#3 Promotes Weight Gain
This one might not surprise you, but the reason might. Sugar-sweetened foods like cookies, candy and flavored yogurts are high in calories but don’t help you feel full. That means you’re often hungry sooner, which can lead to overeating and — over time — unwanted weight gain.
#4 Increases the Risk of Metabolic Syndrome
According to the National Institutes of Health, metabolic syndrome is a group of conditions that collectively raise your risk of heart disease, diabetes and stroke. Excess sugar consumption is closely linked to several of its key markers, including:
- Elevated triglycerides
- Low HDL (good) cholesterol
- High blood pressure
- Increased abdominal fat
#5 Raises Your Risk for Heart Disease
A high-sugar diet can increase several cardiovascular risk factors, like elevated blood pressure, chronic inflammation and unhealthy blood lipid levels. One study found that people who got 17–21% of their daily calories from added sugar had a 38% higher risk of death from heart disease compared to those who kept intake below 8%.
#6 Damages Your Teeth
If you had cavities as a kid, you already know: Sugar isn’t doing your teeth any favors. Oral bacteria feed on sugar and produce acid. If you’re consuming added sugar often, it wears down tooth enamel and causes cavities over time. Sticky candies and sugary drinks are especially problematic.
#7 Causes Sugar Crashes and Low Blood Sugar
You’ve probably heard of a “sugar crash” — but what actually causes it? After consuming added sugar, your blood glucose spikes quickly (high blood sugar). Within two to four hours, it often plummets, leading to reactive hypoglycemia (low blood sugar). This can cause physical symptoms like:
- Dizziness
- Shakiness
- Sweating
- Sudden hunger
Natural Sugar vs. Added Sugar: What You Need to Know
Not all sugar harms your body. In fact, there’s a big difference between the sugar in a fresh apple and the sugar in a piece of apple-flavored candy.
Naturally occurring sugars, like those found in fruit, dairy and some vegetables, come with fiber, vitamins and water. These components slow down how your body absorbs sugar into your bloodstream. This helps prevent blood sugar spikes and gives your body time to process energy more steadily.
Refined or added sugars, on the other hand, are often stripped of nutrients and fiber. They’re quickly digested, which can lead to a rapid rise and crash in blood glucose. That’s why eating a lollipop hits you differently than biting into a banana, even if the sugar grams on the label seem similar.
How to Reduce Sugar Intake (Without Hating Your Life)
Cutting back on sugar doesn’t mean giving up all the things you love. With a few small changes, you can reduce your sugar intake in a way that feels sustainable, not sad.
Here are some easy, low-effort ways to start:
- Add less sugar when baking: Try cutting the sugar in your go-to recipes by half. In many cases, you won’t taste the difference, and neither will your guests.
- Compare nutrition labels: Check the sugar content on items you consume regularly. If a food or drink contains more than 8–10 grams of added sugar per serving, it might be worth swapping for a lower-sugar option.
- Limit sugary drinks: This one’s a game changer. Sugar-sweetened beverages (like soda, sweet tea and flavored lattes) are one of the biggest contributors to excess sugar intake (and many of the conditions listed above). Try switching to no-sugar-added juices, unsweetened tea or flavored sparkling water.
Take the Next Step in Your Health Career
Want to turn your interest in how the body works into a career advantage? The University of Florida offers entirely online graduate programs in medical physiology, anatomy and pharmacology that can help you do just that.
Whether you’re preparing for health-profession school, advancing in healthcare or making a career shift, UF’s online master’s degree and graduate certificate programs give you the scientific foundation to move forward with the flexibility to keep working while you study.
Earn a graduate credential from one of U.S. News’ top-ranked universities and take the next step in your future. Explore our programs, and complete an application when you’re ready.
Sources:
https://www.nhlbi.nih.gov/health/metabolic-syndrome
Depression Symptoms in Men and Women: What Sets Them Apart?
Imagine a dirty bedroom. The bed is unmade, clothes are strewn across the floor and water bottles decorate every surface. You want to clean. You know you should, but you can’t. Where do you start? It’s so overwhelming. Even though you want a clean room more than anything, you can’t bring yourself to do anything.
This is what depression feels like, except it’s not your room that’s messy; it’s your life.
If this scenario hits close to home, you’re not alone. Every year, about 21 million American adults go through life with major depression. It hits differently depending on age, income and life experiences. But today, we’re going to look at how sex and gender shape major depressive disorder.
The Gender Gap in Depression
Depression can start at any age, but the gap in male and female diagnosis widens as kids move through adolescence. Before puberty, boys and girls are diagnosed with depression at nearly the same rate.
Once puberty arrives, young girls struggle with guilt, sadness, trouble concentrating and negative body image. Boys with depression are more likely to lose interest in hobbies and wake up feeling drained.
Symptoms of Depression in Men vs. Women
Individuals of any gender can experience classic signs of depression like:
- Depressed mood
- Trouble thinking, concentrating or making decisions
- Fatigue, lack of energy or feeling slowed down
- Feelings of worthlessness or excessive or inappropriate guilt
- Insomnia or hypersomnia
- Loss of interest in hobbies
- Significant weight loss or gain
- Thoughts of death or suicide
But here’s the thing: The tools for diagnosing depression are based largely on women’s symptoms, since women are diagnosed more often — 16% of women compared to 10.1% of men. So, these classic symptoms mostly describe how depression shows up in women, not necessarily men.
Signs of Depression in Men
For men, depression is far more external. Men are often taught to bottle up their emotions, so when depression surfaces, it can look like:
- Controlling or abusive behavior
- Escapism (like spending a lot of time at work)
- Impulsive anger
- Physical complaints: headaches, stomach issues or neck and back pain
- Risk-taking (like compulsive gambling)
- Substance abuse
Why Male Depression Often Goes Undiagnosed
Because these aren’t the “typical” signs, male depression is often overlooked. Social expectations also push many men to hide their feelings and avoid asking for help, fearing the stigma and discrimination that depression can bring. So, they suffer in silence.
Beyond Biology: The Role of Gender
Biology isn’t the whole story here, however. Consider that the gender gap narrows in populations with greater gender equality, and that gender inequality is associated with higher rates of depression in women.
It’s also men, not women, that are more likely to struggle with depression later in life if they’re single or have less social support. With this perspective, it’s clear that socially constructed roles, not just biological sex, can shape depression.
Types of Depression That Only Affect Women
Women face unique types of depression, particularly during life stages that trigger hormonal changes:
- Premenstrual dysphoric disorder (PMDD) is a severe form of premenstrual syndrome (PMS) with debilitating symptoms like mood swings, irritability, appetite changes, difficulty sleeping, suicidal thoughts and physical symptoms, such as breast tenderness or headaches.
- Perimenopausal depression can affect women during menopause. As if abnormal periods, sleep issues, mood swings and hot flashes weren’t enough, perimenopausal depression can trigger intense anxiety, sadness and loss of enjoyment of life.
- Perinatal depression shows up during pregnancy or after childbirth. Symptoms include feelings of deep sadness and hopelessness as well as trouble bonding with and persistent doubts of caring for the baby.
New dads can go through the “baby blues,” too. Known as paternal postpartum depression, this depressive episode resembles postpartum depression, with symptoms like sadness, frustration and fatigue. Hormonal changes and the stress of parenthood can make anyone vulnerable, regardless of gender.
All in all, if you know some new parents, check up on them and send some well wishes their way (or better yet, a gift card for food delivery).
Men vs. Women: Suicide Risk and Getting Help
Though women are far more likely to experience suicidal thoughts, men are more likely to die by suicide, accounting for eight out of every 10 cases in the U.S. The reason? Men often turn to more lethal methods, like firearms, while women more often choose less deadly means, like poisoning.
Everyone has a hard time admitting they need help. Women are more likely than men to seek help: 43% of women compared to 33.2% of men attend therapy or counseling. But the real takeaway should be that there is help out there, and it actually works.
Where to Find Help for Depression
Talk therapy and medications have helped countless people manage depression and other mental health struggles.
Not sure where to begin? Try the Substance Abuse and Mental Health Services Administration — they’ve got free help and support.
Or check out FindTreatment.gov for local options.
And if you just want to learn more, NAMI (the National Alliance on Mental Illness) has resources that make the maze of mental health a whole lot easier to navigate.
Key Takeaways
Here are a few things worth keeping in mind after this read:
- Do men and women experience depression differently?
Yes. Women experience traditional depression symptoms like sadness, fatigue or loss of interest in hobbies. For men, depression is more external and characterized by anger, escapism and substance abuse.
- Why is depression often overlooked in men?
Male symptoms of depression don’t always align with traditional symptoms, so professionals may not spot the signs. Men also downplay their symptoms and feelings out of fear of being stigmatized.
- What types of depression are unique to women?
Women can experience premenstrual dysphoric disorder (PMDD), perimenopausal depression and perinatal depression, all of which occur during life stages that trigger hormonal changes.
- Can men get postpartum depression?
Yes. New moms and dads alike can feel the “baby blues.” Men going through paternal postpartum depression experience many of the symptoms associated with postpartum depression, including feelings of sadness, frustration and fatigue.
Start Your Journey in Medicine
One person can make a difference — and yes, that person could be you. Whether you dream of treating patients or discovering the next breakthrough drug, your work could transform the lives of people battling mental health challenges.
If you’re ready to dive deeper into the science and care behind conditions like depression, the University of Florida’s online medical sciences programs are your launchpad. Designed for future doctors, physician assistants and pharmacists, our entirely online programs will prepare you for what comes next while giving you the tools to make a real impact in medicine.
Visit our Programs page to learn more!
Sources:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/depression-his-versus-hers
https://pmc.ncbi.nlm.nih.gov/articles/PMC10102695/
https://www.mayoclinic.org/diseases-conditions/depression/in-depth/male-depression/art-20046216
https://www.nimh.nih.gov/health/publications/depression-in-women
The Science Behind Blushing from Embarrassment
Can you think of the last time you felt embarrassed in public? Maybe you tripped over a chair during a work meeting or fumbled your words during a presentation. Whatever the reason, did you feel the telltale signs of embarrassment?
You know the ones: the heat rushing to your cheeks, the increased thump-thump-thumping of your heart and the uncomfortable butterflies in your stomach?
These aren’t just feelings; they’re full-body physiological responses. We’re here to break down why embarrassment produces such a strong physical reaction in so many of us.
Why Does the Body React to Embarrassment?
Our brains perceive embarrassment as a threat to social belonging, which activates the fight-or-flight response via the sympathetic nervous system. But what’s driving all that physiological drama?
Humans are highly social creatures. Whether or not you care what others think, our brains are hardwired to value group acceptance. From an evolutionary standpoint, being rejected by the group once meant losing access to food, safety or protection. While our environments have changed, that deep-rooted instinct hasn’t.
That’s why even minor social slip-ups, like spilling coffee on yourself or tripping in front of a crowd, can trigger real physical symptoms. You might blush, start sweating or even feel your stomach drop. It’s your body’s way of saying: “Hey, this could be important—pay attention!”
Butterflies and Blushing: What’s Happening Internally
In an embarrassing moment, all you care about is making it stop — anything to stop your heart from pounding or your face from heating up. But what’s the science behind why we find ourselves blushing from embarrassment?
Several bodily systems work together to create these uncomfortable physical symptoms. Below, we break it down, one awkward reaction at a time:
Blushing
Embarrassment activates the sympathetic nervous system, causing vasodilation. Your blood vessels begin to dilate, and in uncomfortable situations, you’ll often notice the effects of vasodilation on your face and neck, making those areas visibly red.
Butterflies
Most of us have felt it: a sudden drop in the stomach that feel like butterflies fluttering inside. Other times, it’s more like elephants stampeding to get out. Either way, the sensation is caused by a reduction in digestive activity.
When your brain triggers the fight-or-flight response, your stomach reacts to stress hormones by slowing down digestion. This allows more blood to be rerouted to the lungs and muscles, prepping the body for quick action if needed. That sudden dip in gut activity is what creates the unsettling, fluttery feeling in your stomach.
Increased Heart Rate
An awkward moment might not seem like a true “social threat,” but your brain disagrees. When it triggers your sympathetic nervous system, your adrenal glands respond by releasing adrenaline, which in turn causes your heart rate to increase.
It may seem unnecessary when all you want is for the floor to swallow you whole. However, from an evolutionary standpoint, the increased heart rate is your body’s way of responding to perceived danger (even if that “danger” is accidentally calling your teacher mom in front of the whole class).
Can You Control Embarrassment Responses?
Sadly, no — you can’t control how your body reacts to embarrassing situations. Most physiological responses are autonomic, meaning they happen without conscious effort. Just like you can’t will your pupils to dilate or your heart to beat, your body kicks into embarrassment mode on its own after a bout of social trauma.
However, some coping strategies may reduce the intensity of some of these not-so-pleasant side-effects, like:
- Box breathing
This simple technique slows your breath and signals safety to your nervous system. Try breathing in for five seconds, holding for five, exhaling for five, and holding for five more. Repeat a few times until your breathing and mind begin to calm.
- Reframing
With this technique, you mentally shift your perspective to reduce the perceived threat of the situation. For example, instead of thinking “Everyone saw me trip — how embarrassing!”, try “Everyone trips sometimes. At least I can laugh it off.”
- Practice
As uncomfortable as it might sound, repeated exposure to awkward or high-pressure moments (like public speaking) can desensitize your response over time.
Before you know it, the redness in your cheeks will fade and your racing heart will return to its normal pace, all thanks to the parasympathetic nervous system. Like a built-in reset button, this system slows your heart rate, lowers blood pressure and returns your body to a calm, balanced state after a fight-or-flight response.
Frequently Asked Questions About Embarrassment
Embarrassment is something we all experience. However, few of us stop to wonder why our bodies react the way they do. Below are answers to a few common questions that break down the physiological processes behind those awkward, full-body responses.
- What happens to your body when you’re embarrassed?
Several systems spring into action at once. Blood vessels dilate, causing facial redness. The heart speeds up to pump more blood, and digestion slows down, producing the infamous “butterflies.” All of these are involuntary responses aimed at preparing the body for a perceived threat, even if the “danger” is just tripping over your words in a meeting.
- Why do we care so much about what others think?
Even if you tell yourself not to worry about other people’s opinions, your brain is wired to value group acceptance. From an evolutionary perspective, being part of a group once meant survival. That ancient wiring still influences our emotions today, especially in social situations that feel threatening or high-stakes.
- Can you stop yourself from blushing or feeling butterflies?
Not really. Most of these reactions are controlled by your autonomic nervous system, which means they happen without conscious control. However, techniques like box breathing, cognitive reframing and repeated exposure to stressful situations can help reduce their intensity over time.
Explore the Finer Details of Medical Physiology at UF
Embarrassing moments pass, but neglecting your career goals might lead to some serious discomfort 15 years down the line. Though a graduate credential in medical sciences may seem lofty at first, it’s the first step for many students toward rewarding careers in healthcare, working directly with patients or making an impact behind the scenes.
Not sure which path fits you best? Start by narrowing your options based on your career interests:
- Medical Physiology and Pharmacology: Ideal for future physicians, MCAT prep, biotech professionals or pharmacology researchers
- Medical Physiology and Aging: A strong match for those interested in gerontology, long-term care, health policy or OT/PT preparation
- Anatomical Sciences Education: Best suited for aspiring college instructors, simulation lab professionals or pre-health advisors
- Medical Anatomy and Physiology: A flexible option for those still exploring their path or aiming for medical school
No matter where you’re starting from, there’s an online graduate program that can move you closer to where you want to be. Contact us to learn more about which program might be the best fit for you
Biotechnological Innovations in Tissue Engineering
Ever wish you could just 3D-print a new knee after a long morning run? Thanks to some major breakthroughs in biotechnology, that idea isn’t as farfetched as it once seemed.
Today, the global market for tissue engineering is worth about $20.1 billion, and it’s expected to double by 2033. That growth is fueled by the rising demand for regenerative therapies, advanced procedures and a growing interest in repairing the body in ways once thought impossible.
Let’s look at the most promising innovations being developed in the world of tissue engineering.
What Is 3D Bioprinting?
Remember the replicators from “Star Trek”? “Tea. Earl Grey. Hot.” Today’s versions are a little messier, but they’re surprisingly close to that science fiction version.
A bioprinter works much like a home printer but uses living cells. Researchers use “bioinks” made from stem cells and scaffolding materials to print tissues such as cartilage, skin and even small blood vessels.
Latest Breakthroughs in 3D Bioprinting
Here are some of the latest breakthroughs in 3D bioprinting that are shaping the future of medicine.
- Wake Forest’s Institute for Regenerative Medicine created an ear-shaped cartilage structure that held its shape after implantation in animals.
- The University of Florida created 3D-bioprinted functional liver tissue, moving us closer to full-scale, transplantable organs.
While 3D printing could eliminate the need for donor tissue, reduce transplant rejection and drastically shorten recovery times, one challenge remains: vascularization—keeping printed tissue alive by getting blood and nutrients flowing through it.
Smart Scaffolds: Coaching Cells to Heal
Not every medical solution requires printing from scratch. Sometimes, it’s better to help the body rebuild itself. That’s where smart scaffolds come in.
These tiny 3D structures, made from body-safe materials, are designed to guide cells as they grow and organize. What makes them “smart” is their ability to talk to cells, releasing growth factors and chemical signals that encourage healing. Over time, they dissolve, leaving only new tissue behind.
Latest Breakthroughs in Smart Scaffolding
Here are a few recent breakthroughs in smart scaffolding that are making researchers take notice:
Hydrogel-nanoparticle composites are being studied for nerve regeneration and deep-tissue injury repair, which is paving the way for complex procedures that previously had no good treatment options.
Researchers are also testing chitosan–alginate scaffolds that mimic spinal cord structure to support stem cell growth and nerve repair.
CRISPR and Bioprinting: Using Gene Editing for Stronger Tissues
Imagine fixing a problem before it even exists. CRISPR gene editing acts like a pair of molecular scissors, allowing scientists to snip out faulty genes and replace them with healthy sequences. By editing stem cells before tissue engineering them, scientists can even grow disease-resistant tissues—like fixing a house’s blueprint before setting up the frame.
Latest Breakthroughs in Gene Editing
Here are some of the latest breakthroughs in gene editing worth noting:
- At the University of Florida, scientists are using CRISPR to correct genetic mutations in muscle stem cells, potentially treating disorders like Duchenne muscular dystrophy.
- At the Broad Institute (a leading biotech research center), researchers are combining CRISPR-edited cells with tissue scaffolds to model and potentially treat conditions like heart failure or liver disease.
Organoids: Growing Mini Organs For Drug Testing and Research
What if you could grow a mini version of a liver (or a heart, or lungs) in a lab dish and give someone a second chance at life. Sounds too good to be true, right? But these tiny, functional models called organoids are already in use.
Despite their small size, organoids closely mimic the structure and function of real organs. And because they’re made from a patient’s own cells, they offer a safer, faster way to study diseases, test new drugs and personalize treatment plans.
Latest Breakthroughs in Organoids
Here are some exciting breakthroughs happening in the field of organoid research:
- Researchers at Cincinnati Children’s Hospital used intestinal organoids made from patient cells to test treatments for cystic fibrosis. This helped doctors choose the most effective drug before administering it.
- Novoheart, a biotech company, is growing tiny beating human hearts to better study drug therapies and heart disease.
Microfluidics: Keeping Engineered Tissue Alive
This brings us to a major challenge in tissue engineering: making sure new tissue survives after it’s implanted. Microfluidic systems are tiny, chip-like devices that mimic blood flow and fluid movement. When built into bioprinted tissue, these “mini networks” help keep it alive and growing.
Microfluidic technology is already being tested in things like skin grafts and heart patches. If they work at scale, we may finally have the missing piece to create fully functional lab-grown organs.
Recap: What We’ve Learned and the Big Picture
We’re entering a time when replacing a knee, regenerating nerves or repairing a damaged liver might not involve a long waitlist or a donor. People suffering from organ failure could be saved with their own cells—printed and engineered with precision. These advances will transform how we treat the human body — and save lives.
Let’s recap the technologies we’ve explored:
Key Innovations in Tissue Engineering
- 3D Bioprinting: Printing living tissue using stem-cell-based bioinks.
- Smart scaffolds: Guiding natural tissue regeneration using bioactive, biodegradable structures.
- CRISPR gene editing: Correcting genetic mutations before tissues are even created.
- Organoids: Miniature lab-grown organs used for testing, research and personalized care.
- Microfluidics: Simulating blood flow in engineered tissues to keep them alive and functional.
If you’re in healthcare, research—or you’re just curious!—these innovations are pointing to a future where repairing, replacing or even upgrading human tissue could become routine.
Interested in Innovating the Future of Biotech? Start at UF
Whether you’re fascinated by gene editing, want to design artificial organs or hope to turn your love of biology into real-world impact, it all starts with understanding the human body from the inside out.
The University of Florida’s fully online medical sciences graduate programs are built for people like you: thinkers, doers and future problem-solvers in biotechnology and medicine. Whether you’re pre-med, working in healthcare, pivoting into research or brushing up your skills with a certificate, you’ll gain a deep foundation in human physiology, anatomy, pharmacology and molecular biology in our online programs.
We may not be printing human hearts just yet, but at UF, you’ll be learning how to make that future possible. That journey starts with innovators like you who are passionate about advancing health. Start your journey today and explore our programs!
Sources:
https://pmc.ncbi.nlm.nih.gov/articles/PMC6091336/
https://pmc.ncbi.nlm.nih.gov/articles/PMC7407518/
https://www.numberanalytics.com/blog/future-tissue-engineering-trends-innovations
https://www.nature.com/articles/s41378-024-00759-5
How Do Vaccines Work? A Simple Guide to the Immune System and Immunization
Vaccines save lives. Period.
Take the flu shot. (No, really, take it.) During the 2023-2024 flu season, influenza vaccines prevented:
- 9.8 million flu-related illnesses
- 120,000 hospitalizations
- 7,900 deaths
And that’s just one vaccine. Throughout your life, you’ll likely be vaccinated against as many as 21 dangerous or deadly diseases, including hepatitis B, polio and tetanus. Each shot protects not only you but everyone around you.
But how do vaccines work, exactly? Take a breath (and look away if you have to) while we administer a dose of vaccine knowledge.
First Things First: What Are Vaccines?
A vaccine is a medical treatment that teaches your body how to defend itself against a specific disease — before it even shows up. Vaccines can be administered as a shot, pill, nasal spray or liquid.
How Do Vaccines Work?
To put it simply, vaccines imitate an illness without actually causing the illness.
Vaccines contain either:
- a weakened version of the virus or bacteria, or
- the biological blueprints for producing a harmless piece of it, called an antigen
This antigen triggers an immune response, and your body responds by creating antibodies: proteins that attack foreign substances like bacteria and viruses.
Think of your immune system as a nightclub bouncer. Getting a vaccine is like showing the bouncer (white blood cells) a photo of a known troublemaker (antigen). The next time that troublemaker shows up, they can’t get past the door (antibodies).
An Inside Look at Vaccines and Your Immune System
White blood cells, also called leukocytes, are your body’s defenders. There are five total types of white blood cells, but the three that fight and prevent infection are:
- Macrophages: the body’s alarm system
- T cells: the attackers
- B cells: the antibody factories
Created in your bone marrow, these cells circulate through the blood stream, slipping through blood vessel walls and tissue in search of foreign substances. When one is found, they rally other white blood cells to defend your body.
How Vaccines Trick Your Body Into Making Antibodies
When you receive a vaccine, here’s what happens:
- Macrophages spot the antigen and signal T cells to attack the fake threat.
- Cytotoxic T cells destroy the antigen-infected cells.
- Suppressor T cells prevent other T cells from attacking the body.
- B cells produce targeted antibodies to take down the antigen.
And here’s the important part:
Your body also produces antibody-producing memory cells that can launch a faster, stronger defense next time. Even if you still get sick, vaccines help your body fight back and make the odds of ending up in the hospital (or worse) lower. Way lower.
What Is Full Immunity — and How Do You Get It?
But wait! You might not be immunized yet. A single vaccine dose provides only partial protection, and the number of doses needed to achieve immunization depends on whether the antigen in the vaccine is alive or dead.
- Live-attenuated vaccines (like the one for chickenpox) contain a live, weakened bacteria or viruses. You usually only need one or two doses for lifelong protection.
- Non-live vaccines (like those for influenza and COVID-19) require three or more doses to build up immunity. These viruses mutate quickly, demanding vaccine boosters: updated vaccines for an updated threat.
Why Are Vaccines Important?
Vaccines protect you and your loved ones from preventable diseases. But here’s why vaccines matter even if you feel fine.
Some people can’t get vaccinated, like those with a weakened immune system or a severe allergy to vaccine components. But they can be protected if enough people around them are vaccinated.
This kind of group protection is called herd immunity.
When enough community members are vaccinated or immune, diseases can’t spread as easily. That means fewer outbreaks, fewer hospitalizations and fewer lives lost.
Getting vaccinated is one of the easiest ways to save lives. Honestly, they should hand out medals with every Band-Aid.
Want to Do More Than Just Get the Shot?
While we don’t have a lollipop or colorful bandage to send you away with, we can leave you with sound advice:
If you’re passionate about protecting public health — especially in a time when vaccines and science are constantly under fire — you don’t have to sit on the sidelines.
The University of Florida offers numerous online medical science programs that can help you step up and make a difference, whether you’re interested in medicine, pharmaceuticals or education.
If you’re ready to commit yourself to public health, apply to one of UF’s online medical science programs. Because just like vaccines, one small decision can save lives.
Sources:
https://www.who.int/news-room/feature-stories/detail/how-do-vaccines-work
https://www.cdc.gov/vaccines/basics/explaining-how-vaccines-work.html
https://medlineplus.gov/ency/anatomyvideos/000137.htm
How Deep Can You Scuba Dive? Exploring How Our Bodies Adapt
When you think of scuba diving, one of two things probably comes to mind: the thrill of checking off a bucket list adventure, or the cautionary tales about divers surfacing too fast and getting “the bends.”
Either way, there are likely plenty of questions swimming around your head. How deep can you actually dive? How does your body adjust to being underwater? And what are the real risks you should know about?
We’re here to dive into the answers to all your burning scuba diving FAQs.
How Deep Can a Scuba Diver Go?
Just how far you can venture into the ocean’s depths (or that cenote, quarry or lake you’ve been eyeing) depends on a few key factors, like your diving experience and the environment itself. For most recreational scuba divers, the safe limit is around 130 feet (or 40 meters).
However, some divers go well beyond that. Welcome to the world of technical diving: a more advanced form of scuba that takes you deeper into caves, shipwrecks and other underwater landscapes. Technical divers rely on specialized gas mixtures with specific concentrations of oxygen, nitrogen and helium, carefully calibrated to match the dive’s depth and duration. With this specialized gear and training, they can safely reach depths of up to 330 feet (or 100 meters).
What Happens to Your Body When You Scuba Dive?
With the right equipment, you can dive deep enough to explore endless underwater oases and shipwrecks. But what exactly happens inside your body as you go deeper and return to the surface? Let’s break it down:
- Immersion
As you dive, the pressure pushes blood from your legs to your chest. This makes your heart work harder and can raise your blood pressure. You might notice a heaviness in your chest the deeper you go.
- Pressure
Have you ever swum to the bottom of a deep pool and felt discomfort in your ears? Now, imagine diving eight times deeper.
The deeper you dive, the greater the pressure on your body. This increased pressure affects your sinuses, ears and lungs, which may cause pain and an inability to breathe deeply. Blood flow to your brain also increases, which can intensify sensations of tightness or pressure throughout your body.
- Cold
The deeper you go, the colder the water becomes. As you descend into the cooler water, your blood vessels constrict, causing your heart to work harder to pump blood through them. This increase in pressure can make your body feel cold and stiff.
How Does the Human Body Adapt to Diving?
They rely on the mammalian dive reflex, a natural response seen in all mammals when submerged in water. This reflex kicks in immediately when divers go underwater and hold their breath. It helps conserve oxygen by slowing the heart rate and constricting blood vessels.
The body responds with bradycardia (slower heart rate), apnea (a temporary pause in breathing) and increased blood vessel resistance. This effectively slows the heart’s beats per minute and redirects blood to vital organs, conserving oxygen for essential muscles.
But it’s not all automatic: Divers also train their bodies to adapt to deeper dives and the increased pressure on their lungs. Through specific breathing exercises and lung training techniques, they can improve their oxygen efficiency and increase lung capacity, allowing them to dive deeper and stay submerged for longer.
What Are the Risks of Scuba Diving?
As with any adventure sport, there are risks involved when scuba diving. As mentioned earlier, divers can get decompression sickness (the bends) or other conditions related to increased pressure and gas absorption.
Below, we explain some of the risks of scuba diving:
- Decompression sickness
This occurs when divers ascend too quickly, causing nitrogen bubbles to form in their tissues. Symptoms may include dizziness, joint pain and paralysis — and in severe cases, it can be fatal. The condition earned the nickname “the bends” because the intense bone and joint pain can cause affected divers to double over in excruciating pain.
- Barotrauma
This injury happens when pressure differences between the inside of the body and the surrounding water cause damage. For example, sinus barotrauma occurs when unequal pressure affects the sinuses, leading to pain, nosebleeds or even facial swelling. Other forms of barotrauma may affect the lungs or ears.
- Arterial air embolism
This serious condition results from pulmonary barotrauma: when expanding air becomes trapped in the lungs during ascent. If air bubbles enter the arterial bloodstream, they can block blood flow to vital organs, potentially causing a stroke or heart attack. Divers can reduce the risk by breathing continuously and ascending slowly to avoid lung over-expansion.
- Nitrogen Narcosis
Divers who descend below 100 feet are at risk of nitrogen narcosis, where excess nitrogen under pressure affects the nervous system. This can impair judgment, coordination and decision-making, sometimes giving divers a sensation similar to intoxication.
Explore the Depths of Health Sciences at the University of Florida
Take your passion for health sciences to the next level with flexible online programs designed for working professionals. Whether you’re pursuing a career as a physician assistant, nurse practitioner or medical scientist, the University of Florida offers more than half a dozen online graduate credentials to help you advance toward your career goals.
From a graduate certificate in medical anatomy and physiology to a master’s degree in medical physiology and pharmacology, you can customize your education to match your professional ambitions. And with fully online options, you’ll have the freedom to earn your graduate credential while balancing work and life — at a pace that fits your schedule.
Browse our online programs and take the next step in your health sciences journey.
Sources:
https://oceanexplorer.noaa.gov/technology/technical/technical.html
https://dan.org/health-medicine/health-resource/dive-medical-reference-books/the-heart-diving/basics-of-your-heart-circulatory-system/#affects
https://pubmed.ncbi.nlm.nih.gov/30855833/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11168797
https://pmc.ncbi.nlm.nih.gov/articles/PMC7965165
https://www.ncbi.nlm.nih.gov/books/NBK470304
The Science of Sunlight: Immune System Benefits and Risks Explained
You’ve heard the saying “an apple a day keeps the doctor away.” But what about nature’s other daily remedy, sunlight?
While there may not be a catchy phrase for it, regular, moderate sun exposure plays an important role in supporting your immune system. From vitamin D production to stimulating immune cell activity, the sun can do more than just boost your mood (or your tan).
Of course, all things in moderation, sunlight included. Too much sun can suppress immune function and increase your risk for serious conditions, including skin cancer.
In this article, we’ll break down how sunlight affects your immune system: the benefits, the risks and what future healthcare providers should know about finding the right balance.
How UVA and UVB Rays Affect Your Skin and Immune System
Before diving into the benefits and risks of sun exposure, let’s look at what happens when UV rays hit your skin. Sunlight delivers energy in the form of ultraviolet (UV) radiation, which triggers several biological responses.
There are two main types of UV rays that impact human health:
- Ultraviolet A (UVA)
These rays penetrate deeper into the skin and make up about 95% of the UV radiation that reaches Earth. UVA is responsible for tanning and also contributes to skin aging and wrinkle formation. It can also damage cells by generating free radicals, the unstable molecules that harm DNA, proteins and cell membranes.
- Ultraviolet B (UVB)
UVB rays affect the outermost layer of skin, the epidermis. They’re the main cause of sunburn and can lead to long-term issues like skin cancer. On the positive side, UVB rays also trigger vitamin D production in the skin, a process essential for immune support.
Vitamin D and Immune System Health: The Sunshine Connection
Fun fact: Your body can’t make vitamin D on its own. It relies on outside sources, and one of the most natural forms is sun exposure.
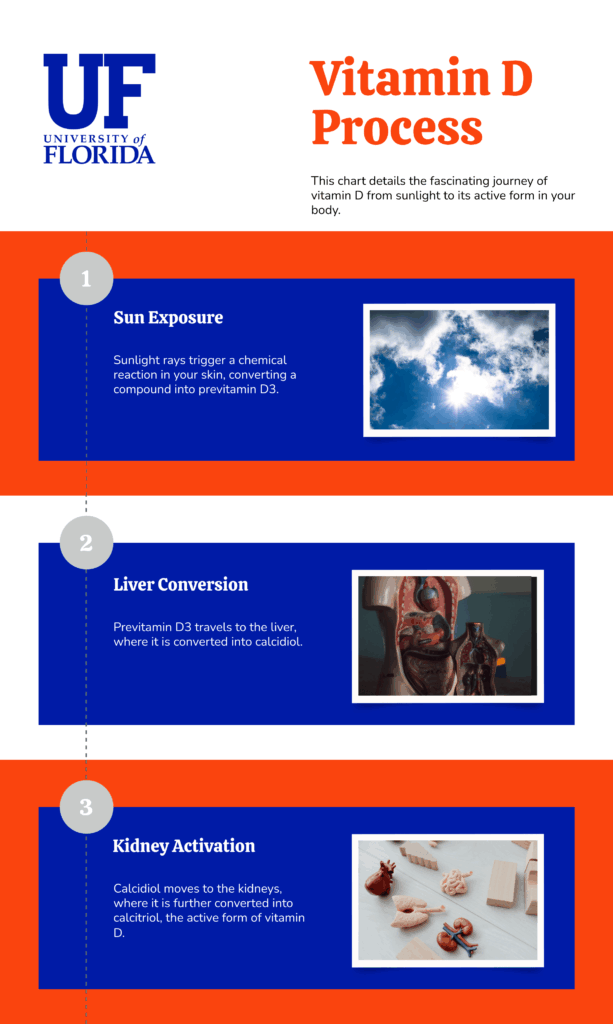
So, how do UVB rays help your body make vitamin D? The infographic below illustrates how sunlight transforms to active vitamin D:
Once converted into its active form, vitamin D plays a crucial role in immune function. It binds to vitamin D receptors in immune cells and helps the immune system in several ways, including:
- Enhancing the body’s first-line defenses (the innate immune system).
- Regulating and calming the second line of defense (the adaptive immune system).
- Reducing the risk of some inflammatory and autoimmune diseases.
Surprising Benefits of Sun Exposure for Your Immune System
Vitamin D synthesis is a well-known benefit of sunlight, but recent studies show sunlight can also enhance your immune function in other ways, including:
- Stimulating antimicrobial peptide production
UVB rays also trigger the production of antimicrobial peptides (AMPs), natural proteins that help neutralize pathogens like viruses and bacteria. These peptides boost the innate immune response by recruiting immune cells to sites of injury and helping wounds heal.
- Enhancing T cell activation with blue light
While the sun may appear yellow or orange, daylight actually contains a full spectrum of colors, including blue light. Blue light helps regulate your circadian rhythm and, according to a 2016 study, may also help T cells (crucial immune cells) respond more quickly to threats.
What Are the Effects of Too Much Sun Exposure?
Sure, a little fun in the sun can support your tanning efforts and give your immune system a boost, but too much of a good thing can backfire. Excessive sun exposure can produce the opposite effect:
- Suppressing immune function
In the short term, too much UVA and UVB can lower your skin’s ability to trigger its innate immune response. Prolonged exposure, however, may raise your risk of infections and reduce your body’s ability to detect and fight cancer cells.
- Damaging cells
Prolonged exposure to UVA and UVB rays can cause DNA mutations, increase inflammation, speed up signs of aging and raise your risk for all types of skin cancer.
Sunlight and Autoimmune Disease: What the Research Shows
Sunlight plays a complex role in autoimmune conditions, offering both potential benefits and risks:
Multiple Sclerosis (MS)
Epidemiological studies suggest that increased sun exposure, particularly during childhood and adolescence, may reduce the risk of developing MS. This protective effect is likely tied to sunlight’s ability to regulate the immune system.
Systemic Lupus Erythematosus
Conversely, for people with lupus, sun exposure can worsen symptoms. UV radiation may trigger skin inflammation and systemic flares, including kidney issues, by activating immune responses that increase inflammation.
Safe Sun Exposure Tips for Immune Support
The sun is unavoidable — and that’s a good thing! Besides prompting vitamin D production and supporting your immune response, it can also improve your mood, help you sleep better and keep your bones in tip-top shape.
So, what’s the sweet spot when it comes to sun exposure?
Aim for 10 to 30 minutes of sunlight per day, depending on several factors:
- Your skin tone
Darker skin tones need more sun exposure to produce adequate vitamin D compared to lighter skin tones.
- Your location
The closer you are to the equator, the more direct sunlight you’ll receive year-round.
- The time of year
During winter months or cloudy weather, your body may need more exposure to achieve the same benefits.
Here are some other tips for safe sun exposure to use when planning your next outdoor activity:
- Use a broad-spectrum sunscreen
For long-term protection, opt for sunscreen with at least SPF 30 that shields against both UVA and UVB rays. Reapply every two hours, or more frequently if you’re swimming or sweating.
- Seek shade during peak hours
UV radiation is strongest between 10 a.m. and 4 p.m. During this time, find shelter under trees, umbrellas or canopies whenever possible.
- Wear protective clothing
Hats, UPF clothing or regular clothes that cover your skin help block direct sun and reduce your risk of sun damage.
Study Human Physiology and Immune Response with UF’s Medical Physiology Programs
Understanding the complex relationship between sunlight, the immune system and overall health is just the beginning. UF’s online graduate programs in medical sciences offer a flexible, in-depth path to explore these topics and more.
Whether you’re pursuing a career as a physician, physical therapist or another health sciences role, our programs are designed with working professionals in mind. Fully online and taught by expert faculty, our programs support your goals without disrupting your schedule.
Explore our online program options to find the right fit for your career path. If you have questions about tuition, start dates or anything else, we’re here to help. We look forward to welcoming you to Gator Nation!
Other articles you may be interested in:
How Does the Immune System Work? 3 Key Strategies
The Aging Process: How and Why We Age
Sources:
https://www.mdanderson.org/publications/focused-on-health/what-s-the-difference-between-uva-and-uvb-rays-.h15-1592991.html
https://pmc.ncbi.nlm.nih.gov/articles/PMC3166406/
https://dermnetnz.org/topics/antimicrobial-peptides
Advancements in Biotechnology for Diabetes Management
Prior to the discovery and use of insulin as a treatment for diabetes in the 1920s, people living with the disease had few treatment options, and essentially no good ones: bloodletting, starvation diets and various potions deceptively marketed as cures.
Today, countless people have been able to bring their diabetes under control through a combination of exercise, dietary adjustments and insulin injections. However, though often effective, these approaches aren’t always practical.
As diabetes management has advanced, new technologies have emerged that address the need for more practical and convenient treatment options. Here we’ll look at some of the current biotechnology helping individuals with diabetes live healthier and less disrupted lives.
Implantable Devices: The Future of Diabetes Care
Continuous Glucose Monitor (CGM)
A CGM assesses the wearer’s glucose every few minutes and tracks this information. These biotechnology devices evaluate the level of glucose in the fluid between cells, not the blood itself, but the numbers are generally comparable.
The device has a small sensor that can be inserted under the skin of the abdomen or arm and kept in place by an adhesive patch. An implantable sensor that goes fully inside the body is also available. Both types of sensors require replacement at regular intervals.
Every CGM has a transmitter that sends glucose data wirelessly to an application on a smartphone, an insulin pump or another receiver device. It’s worth noting, however, that some medicines and vitamins can affect the readings of these devices.
Unnamed Bioelectronic Prototype
Type 1 diabetes causes the body’s immune system to attack islet cells inside the pancreas, impeding its insulin production. A bioelectronic prototype implant device developed at the Massachusetts Institute of Technology, about 1 inch long at its widest dimension, both shields the islet cells from immune system attacks and creates oxygen that preserves the cells long enough to create insulin.
This biotechnology device has some challenges to overcome but shows promise. If viable, it offers the potential to eliminate injections and other tasks associated with managing insulin for Type 1 diabetes patients.
The Artificial Pancreas: Technology Mimicking Nature
Your pancreas creates insulin. But what happens when it doesn’t, as with Type 1 diabetes? A closed loop or “artificial pancreas” can take over that responsibility.
This all-in-one diabetes management system is not like a transplant, where an unhealthy organ is replaced with a healthy one from a donor. Instead, the patient has two devices — a CGM and an insulin pump — attached to the outside of their abdomen.
These devices work in tandem to keep the patient’s insulin at an optimal level. The individual does not need to take any action, as the devices function automatically, allowing them to carry on normal activities without stopping to check or replenish their insulin.
The key difference and benefit between a CGM and a closed-loop system is that the latter uses the data it gathers to automatically deliver the necessary amount of insulin via the insulin pump.
This biotechnology system benefits not only working adults with busy schedules but also children with diabetes who can’t manage the injection regimen themselves or may understandably prefer not to undergo it at all.
Master How Human Body Systems Interact and Respond
UF offers online graduate programs to expand your medical physiology knowledge while preparing for a broad range of rewarding careers. Each program features:
- Affordable tuition.
- No GRE or clinical experience requirements for admission.
- No thesis requirement.
- An asynchronous format that lets you view course lectures at your own pace and maintain your professional and personal commitments.
Master’s Degree in Medical Physiology and Pharmacology
Giving balanced attention to medical physiology and pharmacology, this program offers an in-depth exploration of human body systems and how drugs affect them.
This UF program is ideal for:
- Students preparing for the MCAT.
- Those working or aspiring to work in medicine, pharmacy, pharmacology, drug development, biotechnology or research.
Program details:
- 30 credits
- Can be completed in as little as two semesters.
Master’s Degree in Medical Physiology and Aging
This first-of its-kind degree merges courses from UF’s Graduate Certificate in Medical Physiology and master’s degree in innovative aging studies into a unique curriculum devoted to the biology of aging.
This UF program is ideal for:
- Those working or aspiring to work in medicine, pharmacy, pharmacology, drug development, biotechnology or research careers with an aging or geriatric emphasis.
- Current or future educators and teachers.
Program details:
- 30 credits
- Can be completed in as little as one year.
Graduate Certificate in Medical Physiology
Providing a physiological overview of the major human body systems, this certificate offers a condensed exploration of areas crucial to a variety of professions.
This UF program is ideal for:
- Students preparing for the MCAT.
- Students planning to attend graduate school.
- Practicing professionals looking to add new skills and credentials quickly.
Program details:
- 9-14 credits
- Can be completed in as little as one semester
Benefits of Earning an Online Medical Sciences Graduate Credential With UF
All these programs offer:
- Faculty composed of top researchers, noted academics and MDs.
- International networking opportunities.
- A quality education from an institution ranked among U.S. News & World Report’s:
- Best National Universities
- Top Public Schools
- Best Value Schools
- Best Colleges for Veterans
- Most Innovative Schools
- Top Performers on Social Mobility
Unsure which online graduate medical physiology program matches your needs and goals? We’re here to answer your questions.
Ready to apply? Get started now.
How Hormonal Changes Affect Women’s Mental Health
Ever feel completely off — tired, overwhelmed or emotional — and don’t know why? Your hormones might be to blame. We often think of hormones in terms of fertility, but they also play a crucial role in mental health. Recent research shows that hormonal changes can affect your mood, motivation and cognitive function.
For women, these hormonal shifts are especially significant. As women go through life stages like puberty, pregnancy and menopause, their hormone levels shift in unique ways. This can lead to emotional and cognitive changes that are often misunderstood or misdiagnosed.
Historically, medical research overlooked the impact of women’s hormonal changes, resulting in a lack of understanding about how to effectively support their physical and mental health.
Let’s look at how hormones affect the brain and why understanding them is so important.
How Hormones Affect the Brain
Think of hormones as the body’s chemical text messengers, regulating mood, motivation, memory and behavior by interacting with neurotransmitters like serotonin and dopamine (the “feel-good” chemicals). When hormone levels shift, your emotions often shift with them.
As a result, women are:
- Twice as likely to experience depression.
- Four times more likely to suffer from migraines.
- More likely to die from strokes.
- At earlier risk of alcohol-related brain damage than men.
Estrogen receptors and other female hormones influence mood, reasoning and memory. While men’s testosterone levels also fluctuate, they tend to stay relatively stable compared to the more cyclical hormone patterns in women.
Why Women’s Hormones Affect Mental Health Differently
Many women experience a wave of anxiety, aggression or sadness before their period, a heavy fog or depression after childbirth or brain fuzziness and irritability during menopause. Female hormones like estrogen and progesterone rise and fall in patterns across an approximately 28-day cycle, which is exacerbated by major life events like pregnancy and menopause. These swings can directly impact mental clarity, emotional resilience and even how we process stress.
Cyclical Hormones and Brain Health
Female hormones can double in concentration within 24 hours and shift dramatically throughout the month. These frequent changes make women more vulnerable to anxiety and depression, especially during puberty, pregnancy, postpartum and menopause.
Let’s break down some of the hormones responsible for these shifts.
Key Hormones and Their Roles
- Progesterone: This calming hormone helps regulate the menstrual cycle and supports pregnancy. It also increases GABA, a neurotransmitter that promotes sleep and eases anxiety.
- Estrogen: Estrogen affects much more than reproductive health. It boosts serotonin and dopamine, improves memory and mood, and supports mental clarity.
- Testosterone: Though often called a male hormone, testosterone is important for women, too. It impacts energy levels, motivation, confidence and even spatial thinking.
- Thyroid Hormones: Responsible for your metabolism, these hormones also influence mood, focus and cognitive sharpness. When thyroid levels are off, brain fog and fatigue often follow.
The Diagnosis Gap: Why Women’s Symptoms Are Often Overlooked
Conditions like postpartum depression are frequently underdiagnosed. While it’s normal to experience the “baby blues” after giving birth, persistent sadness, guilt, or emotional disconnection can signal something deeper. In fact, 1 in 7 women experience postpartum depression — and nearly half don’t get the diagnosis or support they need. Hormonal shifts during perimenopause — the years leading up to menopause — can also trigger mood swings, anxiety or depressive episodes. Many women feel “off,” forgetful or mentally foggy, yet these symptoms are often dismissed or misattributed.
So why are women’s symptoms overlooked so often? A key reason is the lack of adequate training in women’s health. A national study found that only 14% of U.S. medical schools offer a dedicated women’s health curriculum. Many OB/GYN residency programs provide little to no education on menopause or hormonal mental health. This gap in medical education leads to missed diagnoses — and too often, to women not being believed when they speak up about what they’re feeling.
How Can We Improve Women’s Healthcare?
The more we understand how hormones affect women’s mental and emotional health, the better care we can offer — not just in crisis, but across every phase of life. Women deserve healthcare that’s informed, personalized and grounded in empathy — whether that’s early intervention for postpartum support, access to hormone therapy, nutritional guidance, and counseling that considers the full spectrum of a woman’s experience. When we bridge the gaps in education and research, we move closer to a system that listens to women, takes their symptoms seriously and supports them holistically. With better knowledge comes better care — beyond one-size-fits-all solutions.
Bridge the Gap in Women’s Healthcare With Medical Sciences
Want to help change women’s healthcare for the better? Understanding how hormones shape brain health isn’t just good science: It’s the foundation for better and more personalized healthcare for everyone. At the University of Florida, our flexible, entirely online graduate programs in medical sciences are designed to help you build that foundation.
Whether you want to explore neurophysiology, endocrine health or anatomy, our programs can prepare you for careers in research, clinical research or healthcare leadership. Choose from our master’s degrees in:
and develop tools to bridge cutting-edge research with real-world impact, improving the diagnosis and treatment of women’s hormonal health.
Looking to brush up your skills? UF also offers online medical sciences graduate certificate programs to stack onto your credentials.
You can be part of a new generation committed to compassionate, research-informed care. Explore UF’s medical sciences programs and discover your path to making a difference.
Sources:
https://www.webmd.com/women/ss/slideshow-hormone-imbalance
https://www.kernodle.com/obgyn_blog/how-types-of-hormones-affect-your-health/
https://www.technologynetworks.com/neuroscience/articles/from-menstruation-to-menopause-how-hormonal-shifts-shape-womens-brain-health-392016
https://www.morelandobgyn.com/blog/womens-hormones-the-main-culprits-for-changes-in-your-health